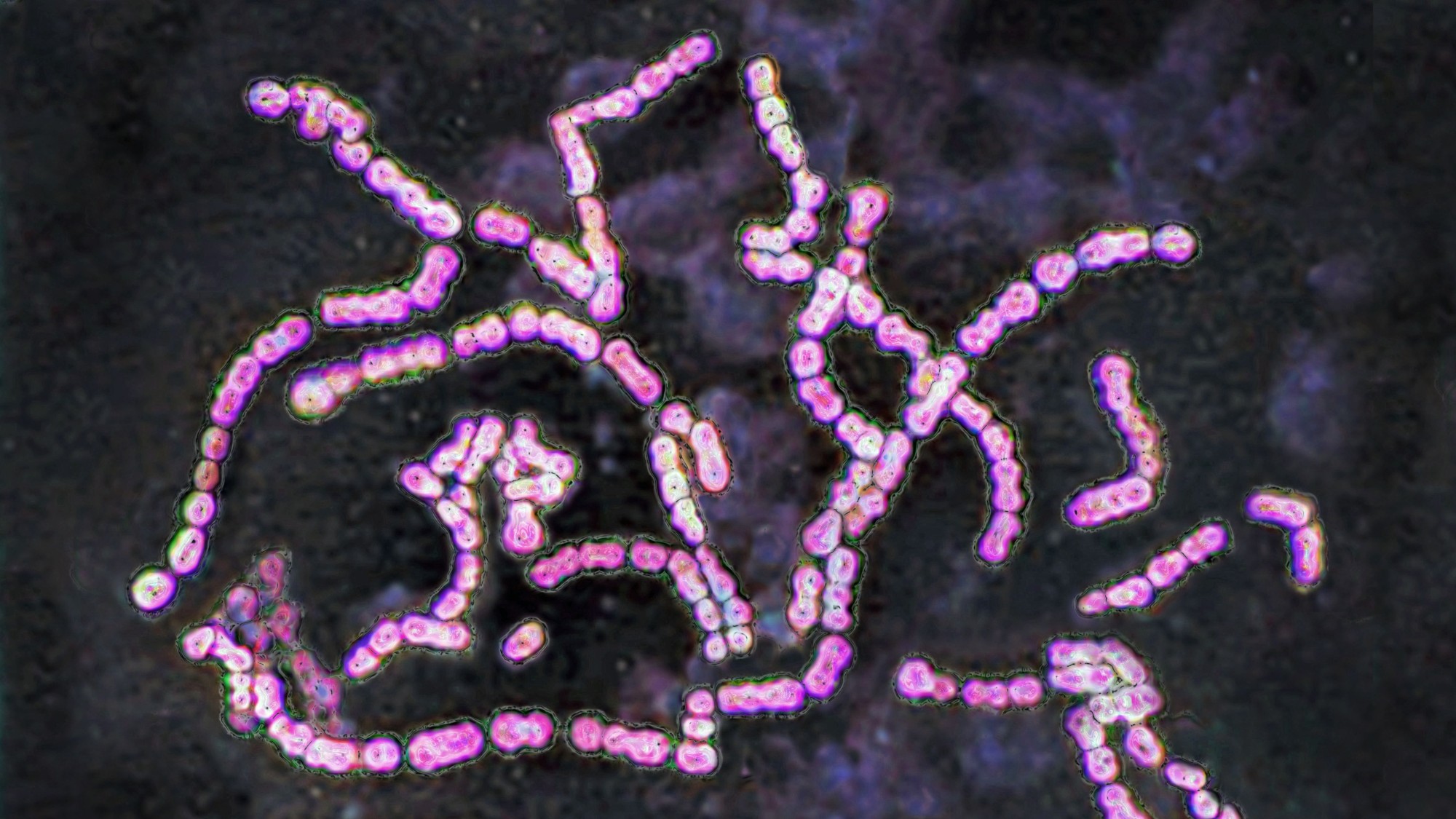
Unseen Threat: The Surge of Strep Infections Across the U.S.
Health officials are sounding the alarm as cases of streptococcal (strep) infections surge unexpectedly across the United States. Hospitals and clinics from New York to California report a sharp rise in both common strep throat and invasive Group A Streptococcus (iGAS) infections, some leading to severe complications. The uptick, first noted in late 2023, has persisted into 2024, raising concerns about antibiotic resistance, delayed diagnoses, and strained healthcare resources. Experts urge the public to recognize symptoms early and seek prompt treatment to curb the spread.
Why Strep Infections Are Spreading Rapidly
The Centers for Disease Control and Prevention (CDC) estimates a 28% increase in invasive strep cases compared to pre-pandemic levels, with pediatric hospitalizations climbing fastest. Dr. Alicia Monroe, an infectious disease specialist at Johns Hopkins, attributes the spike to multiple factors:
- Post-pandemic social mixing: Reduced immunity after years of masking and distancing.
- Antibiotic overuse: Some strains show resistance to first-line treatments like penicillin.
- Seasonal anomalies: Warmer winters have extended strep’s typical November–April season.
“This isn’t just a bad year for sore throats,” warns Dr. Monroe. “We’re seeing more cases of necrotizing fasciitis and streptococcal toxic shock syndrome—conditions that can turn deadly within hours.”
Hotspots and High-Risk Populations
Data from the CDC highlights regional disparities, with the Midwest and Northeast experiencing the highest infection rates. Schools and long-term care facilities have become outbreak epicenters due to close quarters and asymptomatic carriers. Children aged 5–15 and adults over 65 are most vulnerable, but healthy adults are also at risk. In Chicago, a cluster of iGAS cases linked to a single daycare resulted in two fatalities last month.
“Strep A is a shape-shifter,” explains microbiologist Dr. Raj Patel. “It evolves quickly, and milder infections can escalate if ignored. We’ve identified three new substrains this year alone.”
Symptoms and the Danger of Misdiagnosis
Early strep throat symptoms—fever, swollen tonsils, and pain when swallowing—often mimic viral illnesses. However, unlike colds, strep rarely causes coughing or runny noses. Rapid antigen tests can confirm cases, but false negatives occur 15–20% of the time, per a 2023 Journal of Clinical Microbiology study. Left untreated, strep can trigger rheumatic fever or kidney inflammation.
Pediatrician Dr. Lisa Chen recounts a recent case: “A 10-year-old patient presented with fatigue and a mild rash. By the time bloodwork confirmed strep, her organs were failing. Parents must trust their instincts—if something feels ‘off,’ push for further testing.”
Public Health Response and Prevention Strategies
The CDC has issued updated treatment guidelines emphasizing narrower-spectrum antibiotics to combat resistance. Meanwhile, schools in Ohio and Massachusetts now mandate 24-hour symptom-free periods before students return post-illness. Vaccine development remains in early stages, though Moderna announced Phase I trials for an mRNA-based strep A vaccine last January.
Preventative measures include:
- Frequent handwashing with soap, especially after coughing or sneezing
- Avoiding shared utensils or drinks
- Replacing toothbrushes after a strep diagnosis
What’s Next: A Call for Vigilance
While strep infections are historically common, their rising severity demands attention. Health departments are expanding surveillance, and the World Health Organization added iGAS to its priority pathogen list in 2024. For now, experts stress education as the best defense.
“This isn’t about panic—it’s about preparedness,” says Dr. Monroe. “Know the signs, act fast, and advocate for yourself in medical settings.” Readers concerned about symptoms should contact their healthcare provider immediately or visit the CDC’s strep information portal for real-time updates.
See more WebMD Network